Lyme Disease Not Carried by Lone Star Ticks

It now appears lone star ticks have been falsely accused of passing Lyme disease to humans for many years.
Often presumed guilty by association, a new review of 30 years' worth of literature, shows that the lone star tick is not capable of spreading to humans the bacteria that causes Lyme disease.
This new review of 60 different studies tested for transmission of B. burgdorferi by lone star ticks and the tick transmission was never observed.
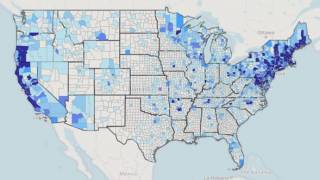
Those studies, encompassing tests on over 52,000 lone star ticks from 22 states by more than 35 research groups, lack convincing evidence that lone star ticks are spreading bacteria that cause Lyme disease, according to the authors.
Moreover, one study determined that the saliva from lone star ticks actually kills the Lyme disease bacteria.
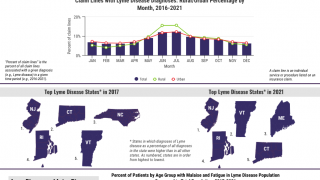
“Debunking the perception that lone star ticks can transmit Lyme disease is important because imprecise inferences about the geographical distribution of infected ticks can have negative public health consequences,” says Robyn Nadolny, Ph.D., biologist and program coordinator at the U.S. Army Public Health Center Tick-Borne Disease Laboratory and co-author of the review.
“The media coverage of Lyme disease might make many Americans think that a tick-bite means only one thing: Lyme disease,” Dr. Nadolny said.
"Lone star tick saliva is a very effective barrier against B. burgdorferi—it literally explodes them," said Graham Hickling, Ph.D., a tick researcher from the University of Tennessee who contributed to the review.
"Lone star ticks are constantly being exposed to B. burgdorferi as they feed on infected animals, but the bacteria species has never been cultured from a Lone Star tick in a lab.”
“However, it has been cultured from rodents and black-legged ticks in the Southeast," said Dr. Hickling.
Lone star tick bites can indeed cause a range of human illnesses, including ehrlichiosis, Southern Tick-Associated Rash Illness (STARI), and red meat allergy.
These authors said that early literature detecting B. burgdorferi in lone star ticks used methods that were not Borrelia species-specific, and any spirochetes that were detected were likely other species.
Advancements in molecular analysis strongly suggest that reports of B. burgdorferi in A. americanum had misidentified B. lonestar.
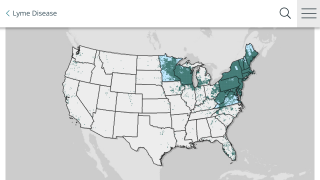
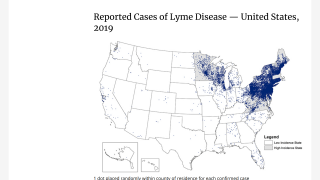
The bacteria that cause Lyme disease, the most commonly reported vector-borne illness in the United States, are transmitted to humans primarily by the black-legged tick (Ixodes scapularis, also known as deer ticks.
Deer ticks are abundant in the eastern parts of the United States.
However, many people produce similar "cross-reactive" antibodies in response to other bacteria not associated with Lyme disease.
This causes confusing results and makes test accuracy more difficult.
The only FDA-approved Lyme disease tests available today was developed more than two decades ago.
The FDA currently recommends a two-tiered testing approach: a conventional enzyme-linked immunoassay (ELISA) test, followed by a Western Blot test.
In a new analysis from Rutgers University, Harvard University, Yale University, and the National Institute of Allergy and Infectious Diseases of the NIH say new diagnostic methods offer a better chance of detecting infection from the Lyme bacteria.
These researchers did not disclose any conflicts of interest: Ellen Y Stromdahl, Robyn M Nadolny, Graham J Hickling, Sarah A Hamer, Nicholas H Ogden, Cory Casal, Garrett A Heck, Jennifer A Gibbons, Taylor F Cremeans, Mark A Pilgard.
Our Trust Standards: Medical Advisory Committee