HIV Vaccine Roadmap Becomes Clearer

Over the years, numerous scientists have stated to 'successfully produce a Human Immunodeficiency Virus (HIV-1) vaccine, innovative technologies could be required.'
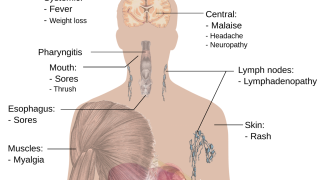
HIV-1 is the most common virus type, has unprecedented genetic variability, and the ability to quickly establish a lifelong infection are just some of the obstacles researchers face in trying to understand how to induce protective immunity against the virus, confirms the International AIDS Vaccine Initiative.
"Finding an HIV (prevention) vaccine has proven a daunting scientific challenge," stated Anthony S. Fauci, M.D. NIAID director, on March 14, 2022.
Most importantly, 'HIV vaccine candidates can not cause HIV infection.'
Since nobody with HIV has ever developed an immune response that cleared the infection, scientists do not yet know what constitutes an effective immune response to the virus, wrote the U.S. NIAID.
However, a new, pre-human study published by the peer-review journal Science Translational Medicines on September 7, 2022, offers a clinical path for accelerating HIV vaccine development.
The extensive research team noted that HIV vaccine candidates tend to focus on empowering the human body to produce antibodies that bind to certain parts of the virus.
The challenge with this approach is that HIV changes its spike protein so quickly.
That means a successful HIV vaccine must target multiple neutralizing antibodies (nAbs) that cover a broad spectrum of proteins.
These researchers wrote, 'A successful HIV-1 vaccine will require induction of a polyclonal neutralizing antibody (nAb) response, yet vaccine-mediated induction of such a response in primates remains a challenge.
We found a stabilized HIV-1 CH505 envelope (Env) trimer formulated with a Toll-like receptor 7/8 agonist-induced potent HIV-1 polyclonal nAbs correlated with protection from homologous simian-human immunodeficiency virus (SHIV) infection.
Structural analyses of vaccine-induced nAbs demonstrated targeting of the Env CD4 binding site or the N156 glycan and the third variable loop base.
CH505 viral isolated mutated the V1 to escape the infection- and vaccine-induced antibodies were isolated.
In summary, these results define the specificities of a vaccine-induced nAb response and the protective titers of HIV-1 vaccine-induced nAbs required to protect nonhuman primates from low-dose mucosal challenge by SHIVs bearing a primary transmitted/founder Env.'
Regarding a therapeutic HIV vaccine to treat active virus infections, Research Priorities for an HIV Cure: International AIDS Society Global Scientific Strategy was published in Nature Medicine in December 2021.
This strategy identified a series of questions to draw nearer to an HIV cure that must be safe, affordable, and applicable at scale to everyone with HIV.
This research work was supported by the National Institutes of Health Division of AIDS for the Center for HIV/AIDS Vaccine Immunology-Immunogen Discovery, the National Institutes of Health Division of AIDS grant for the Duke Consortia for HIV/AIDS Vaccine Development, and the National Institutes of Health Division of AIDS grant. These researchers disclosed no significant industry-related conflicts of interest.
Additional HIV vaccine development news is posted at PrecisionVaccinations.com/HIV.
PrecisionVaccinations publishes fact-checked, research-based HIV vaccine news curated for mobile readership.
Our Trust Standards: Medical Advisory Committee
- IAVI HIV vaccines
- NIH HIV vaccine studies
- Stabilized HIV-1 envelope immunization induces neutralizing antibodies to the CD4bs and protects macaques against mucosal infect
- NIAID HIV vaccine overview
- Research priorities for an HIV cure: International AIDS Society Global Scientific Strategy 2021
- HIV vaccine candidates