University of Chicago’s Malaria Vaccine Shows Greater Immune & Antibody Responses

Researchers at the Institute for Molecular Engineering at the University of Chicago have developed a new system for delivering a malaria vaccine that shows promise in being much more effective than the current system.
Though a vaccine for malaria exists, RTS,S/AS01 is only effective in 30 to 50 percent of patients, says the World Health Organization.
By developing a vaccine that targets specific cells in the immune system, these UC researchers have seen a much greater immune and antibody response to the new vaccine.
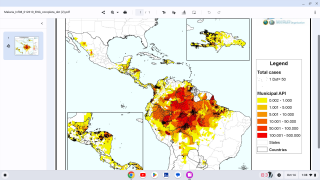
This is important news since malaria remains responsible for nearly 500,000 deaths annually, according to the Centers for Disease Control and Prevention (CDC).
The CDC publishes various travel alerts since millions of US residents travel to countries where malaria is present. About 1,700 cases of malaria are diagnosed in the United States annually, mostly in returned travelers.
“When compared to the current malaria vaccine option, our results are extremely exciting,” said Jeffrey Hubbell, Eugene Bell Professor in Tissue Engineering and corresponding author on this paper, in a press release.
Hubbell and his colleagues developed a vaccine platform made up of a polymeric adjuvant, which contains multiple adjuvant molecules connected like pearls in a necklace, coupled with an antigen.
This vaccine platform can easily drain into the secondary lymphoid tissues and deliver the vaccine to specific cells that make up the body’s immune system.
To make sure it found its way to the intended site, they incorporated mannose, a type of sugar, into the polymeric adjuvant.
Because viruses and bacteria tend to have a lot of sugar on their surfaces, the dendritic cells in the lymphoid tissues have several sugar receptors that help in the recognition of pathogens.
So once the mannose-laden vaccine is injected into the body, it targets specific immune cells, called dendritic cells, which in turn activate T cells.
By specifically targeting dendritic cells, this new technology prevents systemic inflammation while efficiently activating an immune response.
“It’s a targeting material, but it is also inherently therapeutic,” said D. Scott Wilson, a postdoctoral researcher in Hubbell’s lab.
When tested, the vaccine system had a higher antibody response than the malaria vaccine currently on the market. It also provided a cellular response — clearing the infected cells — which the current vaccine does not do.
RTS,S/AS01 is the first, and to date, the only vaccine to show a protective effect against malaria among young children in a Phase 3 trial.
Beginning in 2019, RTS,S/AS01 will be the first malaria vaccine provided to young children through routine immunization programmes.
Researchers have now partnered with Emory University to continue testing the system.
Other authors on the paper include Melody Swartz, William B. Ogden Professor; students Michal Raczy and Ruyi Wang; senior scientist Marcin Kwissa; postdoctoral researcher Maria Broggi; Sachiko Hirosue, Laura Jeanbart, Giacomo Diaceri, Xavier Quaglia-Thermes of the École Polytechnique Fédérale de Lausanne; and Leonardo Bonilla-Ramirez, Jean-Francois Franetich, and Dominique Mazier of the Centre d'Immunologie et des Maladies Infectieuses.
Funding for this research was from Whitaker Foundation, School of Life Sciences EPFL, and the University of Chicago.
Our Trust Standards: Medical Advisory Committee