Why Was the Maternal RSV Vaccine Study Stopped

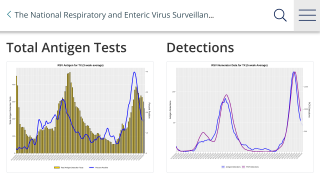
Recently, a clinical trial enrollment was stopped ahead of schedule because of safety concerns. The trial's early findings indicated that the risk of severe lower respiratory tract disease in infants caused by the respiratory syncytial virus (RSV) was lower with the maternal vaccine candidate than with the placebo.
However, the risk of preterm birth was found to be higher with the candidate vaccine.
Published by The New England Journal of Medicine (NEJM) in March 2024, the RSV Prefusion F Protein–Based Maternal Vaccine — Preterm Birth and Other Outcomes phase 3 study (NCT04605159) focused on efficacy and safety data on GSK's RSVPreF3-Mat RSV prefusion F protein-based maternal vaccine candidate involving more than 5,000 pregnant people and their infants in 24 countries.
"We have discontinued our work on this RSV maternal candidate vaccine, and we are closing out all ongoing trials except the MAT-015 follow-on study to monitor subsequent pregnancies," a GSK spokesperson announced.
According to an editorial published by The NEJM on April 12, 2024, the vaccine candidate given during pregnancy was about 66% effective at protecting against RSV-associated respiratory illness and about 69% effective at protecting against severe disease.
However, Emily Harris explained that the researchers had stopped the trial early because of an increased risk of preterm births.
About 7% of infants whose birthing mothers had received the vaccine were born before 37 weeks, compared with roughly 5% of infants whose mothers had received a placebo.
The researchers noted that the higher rate of preterm births was "predominantly observed" among low- and middle-income countries and was not explained by SARS-CoV-2 coronavirus infection or COVID-19 vaccination.
"We have discontinued our work on this RSV maternal candidate vaccine, and we are closing out all ongoing trials except the MAT-015 follow-on study to monitor subsequent pregnancies," a GSK spokesperson informed Medscape in March 2024.
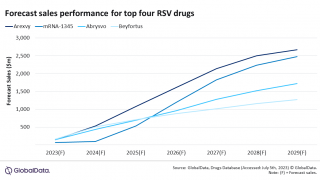
The maternal vaccine evaluated in the study is similar to Pfizer Inc.'s ABRYSVO™, which the U.S. Food and Drug Administration (FDA) approved in 2023 to protect against RSV in infants. The FDA-approved vaccine is being monitored for vaccine-associated risks, including preterm births.
Despite the potential risks of maternal RSV vaccination, "it is essential to weigh this small risk against the proven benefits," the authors of a linked editorial wrote.
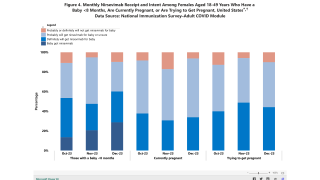
The U.S. CDC's RSVVaxView reported that, as of 2024, the overall RSV vaccination rate among pregnant women was about 18%.
Similar to a vaccine, a single-dose, extended half-life monoclonal antibody has been approved to offer passive immunization to prevent lower respiratory tract infections in children caused by RSV.
According to recent research, BEYFORTUS™ (Nirsevimab) is about 90% (95% CI = 75%–96%) protective against RSV-associated hospitalization in infants in their first RSV season.
As of February 2024, the CDC reported that about 43% of women with infants under eight months had received nirsevimab.
Our Trust Standards: Medical Advisory Committee