Hepatitis E Expands From Pigs to Humans

The Hepatitis E Virus (HEV) gets little press compared to its more popular cousins, Hep A, B and C. But, virologists say we should be on alert for how this virus is changing.
While rare in the United States, the World Health Organization (WHO) reports that Hepatitis E virus infections are the most common cause of acute viral hepatitis worldwide.
The infection usually resolves within weeks, but sometimes causes acute liver failure, which may be fatal.
Historically, HEV transmission was primarily zoonotic in industrialized countries, and by fecal–oral transmission in developing countries, due to poor sanitation.
That picture is starting to change.
Scientists have begun noticing a shift from hepatitis E as only a disease of the poor, to one that can also affect affluent people in developed world settings.
Researchers say people are acquiring the HEV infection from pigs and pork products in countries like the United Kingdom and France.
As an example, in England, an un-named supermarket may have infected thousands of people with the Hepatitis E virus by selling imported pork.
According to new research, pork imported from Europe might be transmitting the virus and infecting between 150,000 and 200,000 British people a year with the virus.
Additionally, a team of French researchers identified rabbit HEV in a small number of human patients who were infected with HEV. These researchers could not identify the source of HEV3-ra infection, given that none of the patients infected with this subtype had direct contact with a rabbit.
Interestingly, several of these HEV3-ra infected patients ate rabbit meat, but the meat was reported to be well cooked.
Such findings, the researchers wrote, “emphasize the zoonotic risk for HEV3-ra and expand the spectrum of potential sources of human infection.”
Complicating the picture further is the fact that HEV is not limited to pigs as hosts. Meat from wild boar and other game animals may also be tainted with the virus, as may seafood items.
Dr Tongai Maponga, a post-doctoral fellow in the Division of Medical Virology at Stellenbosch University, says: "HEV has the potential to become a chronic infection, especially in immunosuppressed patients.’
Of the 5 HEV genotypes infecting humans, HEV3 is the most prevalent. It spreads to humans through direct contact with infected pigs as well as through food and environmental contamination.
The HEV3 genotype has 3 subtypes. Two are found in humans and pigs; the third subtype, HEV3-ra, is found in rabbits. To date, only 1 study has reported a human HEV3-ra infection, reflecting the relatively unknown contribution of HEV3-ra to human HEV infection.
Human HEV3 infections are rare, potentially because humans eat far less rabbit than pork.
According to the WHO, every year, there are an estimated 20 million HEV infections worldwide, leading to an estimated 3.3 million symptomatic cases of hepatitis E. WHO estimates that hepatitis E caused approximately 44,000 deaths in 2015.
Which means, Hepatitis E accounts for 3.3% of the mortality due to all hepatitis cases.
There is no specific treatment capable of altering the course of acute hepatitis E. As the disease is usually self-limiting, hospitalization is generally not required.
Immunosuppressed people with chronic hepatitis E benefit from specific treatment using ribavirin, an antiviral drug. In some specific situations, interferon has also been used successfully, according to the WHO.
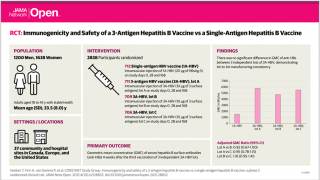
No FDA-approved vaccine for Hepatitis E is currently available in the United States. However, in 2011, a recombinant subunit vaccine to prevent hepatitis E virus infection was registered in China. It has not yet been approved in other countries.
Our Trust Standards: Medical Advisory Committee
- Rabbit Hepatitis E Virus Infections in Humans, France
- Hepatitis E
- Should we be worried about hepatitis E?
- Thousands at risk of pig virus from ‘Supermarket X’ sausages
- Hepatitis E FAQs for Health Professionals
- Pork products associated with human infection caused by an emerging phylotype of hepatitis E virus in England and Wales