Untreated Drinking Water Is a Diminishing Hepatitis A Risk

A new report says people who are unvaccinated for the Hepatitis A virus have another risk to avoid…. drinking untreated water.
This Centers for Disease Control and Prevention (CDC) report published on Septemeber 6, 2019, says ‘public health officials should increase the awareness of Hepatitis A virus (HAV) risks that are associated with untreated groundwater from private wells.’
Although drinking water–associated hepatitis A outbreaks in the United States are rarely reported, the CDC says ‘the HAV can remain infectious in water for months.’
But, the actual health risk may be limited.
This CDC report found 32 drinking water–associated hepatitis A outbreaks in 18 states during 1971–2017, with the last one occurring in 2009.
The most commonly reported water system type associated with an HAV outbreak was individual, accounting for 41 percent of outbreaks, followed by community outbreaks with 31 percent.
Furthermore, all individual water systems with HAV outbreaks were supplied by private wells or springs.
The reasons for the decline in water–associated HAV outbreaks, which have essentially stopped, are increased hepatitis A vaccinations, combined with government regulations that require testing and, where necessary, corrective actions for drinking water supplies.
While the risk of hepatitis A from drinking water has diminished, there are several known risk factors contributing to the ongoing HAV outbreak.
As of September 6, 2019, there have been 25,484 hepatitis A cases reported to the CDC since 2016.
The CDC says ‘person to person’ interactions are the reason behind the outbreak in the USA.
>> Fast test for Hep A <<
Since Hepatitis A is a liver infection caused by a virus, which can be easily spread, the following groups are at highest risk for acquiring an HAV infection:
- People who use drugs (injection or non-injection)
- People experiencing unstable housing or homelessness
- Men who have sex with men (MSM)
- People who are currently or were recently incarcerated
- People with chronic liver disease, including cirrhosis, hepatitis B, or hepatitis C.
Additionally, some states, such as Florida, Ohio, and Tennessee are encouraging ‘food-service’ staff to be vaccinated to reduce the risk of spreading hepatitis A in restaurants.
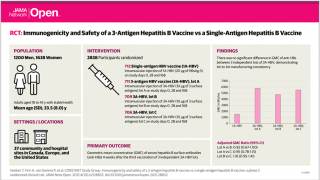
The CDC says just 1-dose of the single-antigen hepatitis A vaccine provides up to 95 percent seroprotection in healthy individuals for up to 11 years.
And, pre-vaccination serologic testing is not required to administer the hepatitis A vaccine.
There are 3 HAV vaccines approved in the USA: Vaqta, Havrix, and Twinrix, which are available at pharmacies in most states.
Furthermore, immune globulin can provide short-term protection against hepatitis A, both pre- and post-exposure.
Any vaccine can cause side effects, which should be reported to a healthcare provider or the CDC.
This CDC report was compiled by Elyse Phillips, Allison D. Miller, Division of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases, CDC. The corresponding author: Catherine E. Barrett, [email protected], 404-718-7664.
Vaccine News Published by Precision Vaccinations
Our Trust Standards: Medical Advisory Committee
- CDC: Impact of Public Health Interventions on Drinking Water–Associated Outbreaks of Hepatitis A — United States, 1971–2017
- CDC: Widespread person-to-person outbreaks of hepatitis A across the United States
- CDC: Frequently Asked Questions: Hepatitis A outbreaks
- CDC: Food Worker Handwashing and Restaurant Factors