Intrahousehold Flu Infections Increased During the Pandemic

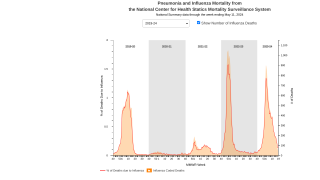
While Influenza virus infections declined globally during the early days of the COVID-19 pandemic, a recent study found an increased risk of household transmission of influenza A(H3N2) in the 2021-2022 flu season compared with prepandemic seasons.
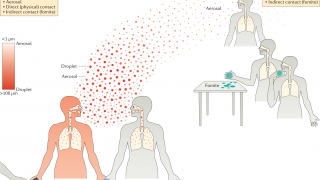
More frequent interaction with an infected person would be expected to increase infection risk, and in 2021-2022, household contacts reported spending more time in the same room with others.
During the 2021-2022 influenza season, once the household knew a person had caught the flu, household contacts continued to report frequent interaction.
In this Original Investigation published by The JAMA Network on January 28, 2023, about 50% of household contacts of patients with influenza were infected in 2021-2022 compared with just 20% of household contacts during influenza seasons before the COVID-19 pandemic.
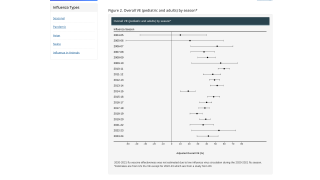
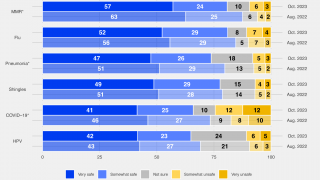
Additionally, this study found the influenza infection rate during the 2021-2022 season was 40.0% among people who received an influenza vaccine during the flu season compared with 58.4% among people who did not receive an influenza vaccine during the 2021-2022 season.
There are several potential reasons that the risk of intrahousehold influenza virus infection during the 2021-2022 season was higher than in previous seasons.
First, antibodies against influenza, whether naturally acquired or vaccine-induced, may have declined or waned over three years since the last time the U.S. population was widely exposed to A(H3N2) viruses in 2018-2019.
Seroprevalence studies suggested that approximately 14% of antibodies acquired from infection wane within a year. Therefore, during years without substantial population exposure, antibody titers could be considerably lower than initial levels.
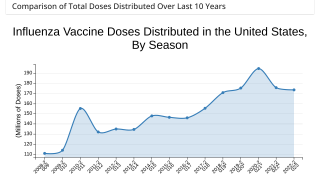
Second, reductions in seasonal influenza vaccination during the COVID-19 pandemic may have contributed to increased population susceptibility.
While influenza vaccination has been relatively stable since 2019, with approximately 55% of people receiving a flu shot during the 2021-2022 season, there were lower vaccination rates among children, and there may have been individual-level changes in vaccination behavior not measured by population-level surveys.
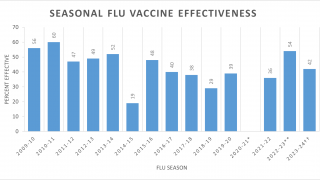
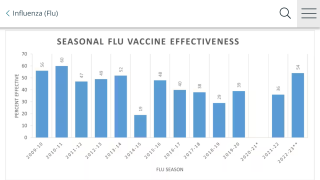
Third, the match between the virus antigens in the annual vaccine and circulating influenza viruses can affect the incidence of seasonal influenza.
The A(H3N2) viruses that circulated during the 2021-2022 season were from a genetic subgroup (3C.2a1b.2a.2, referred to as 2a.2 viruses) that emerged early in 2021 and were antigenically drifted from the A(H3N2) virus included in the 2021-2022 northern hemisphere influenza vaccine.
While laboratory studies show that the 2a.2 viruses may evade neutralization by vaccine-induced antibodies, there was evidence that influenza vaccination during the 2021-2022 season was associated with lower odds of an individual seeking outpatient medical care for an illness by 35%, similar to vaccine effectiveness estimates in prior seasons predominated by influenza A(H3N2) viruses.
Furthermore, patterns of population mixing have also changed over the COVID-19 pandemic, with people generally spending more time at home.
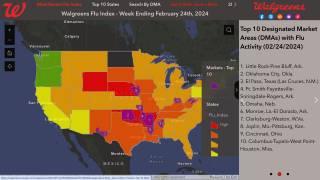
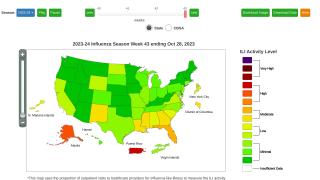
This study's insights remain essential in 2023 as the current flu season continues impacting most families in the U.S.
As of January 14, 2023, data indicates about 171 million influenza vaccines had been distributed for the 2022-2023 flu season. Last flu season, about 174.9 million vaccines were distributed in the U.S.
This study has several limitations, such as households not reflecting changes in contact patterns in the community and/or work settings. In addition, no industry conflicts of interest were disclosed.
Our Trust Standards: Medical Advisory Committee