Minnesota’s Hepatitis A Outbreak Costs May Exceed $100,000

The Minnesota Department of Health (MDH) declared an outbreak of the hepatitis A virus in 9 counties.
The MDH announcement on August 8, 2019, includes 23 hepatitis A cases. Thirteen of these infected individuals were hospitalized for treatment and all have been discharged.
While initial hepatitis A cases were clustered in east-central Minnesota, the infection source is not known for some cases, suggesting some community transmission among high-risk groups of people.
Even though hepatitis A disease burden in the United States has been very low, there still remains a substantial direct and indirect cost burden when treating hepatitis A patients.
Various studies have concluded the average annual cost for treating hospitalized hepatitis A patients covered under commercial health insurance plans could run up to $11,479.
The study found hepatitis A patients over a 12-month study period had more frequent hospitalizations and emergency department visits, and averaged higher utilization of outpatient services.
When using this 2012 data published in the journal Health Outcomes Research in Medicine, the current Minneapolis hepatitis A outbreak will generate over (13 hospitalizations x $11,479) $100,000 in annual expenses.
Minnesota joins several states which have also declared hepatitis A outbreaks in 2019, such as Florida and Ohio.
In May 2019, Minnesota began seeing an increase in hepatitis A cases. These cases had similar risk factors to national outbreaks of hepatitis A that have been occurring.
Since the outbreaks were first identified in 2016, 29 states have publicly reported the following cases to the Centers for Disease Control and Prevention (CDC), as of August 2, 2019:
- Cases: 23,638
- Hospitalizations: 60%
- Deaths: 233
Kris Ehresmann, infectious disease director for MDH, said in a press release, “Declaring an outbreak is a significant step because it allows us to access additional resources to fight the outbreak.”
Hepatitis A is a contagious liver infection caused by a virus. It can range from a mild infection with no symptoms lasting a few weeks to a severe illness lasting several months that can result in liver failure and death, says MDH.
Hepatitis A is usually spread person-to-person when someone unknowingly eats food, drinks a beverage or places an object in their mouth that has been contaminated with microscopic, trace amounts of the virus.
Foodservice workers have been identified as the source for numerous hepatitis A outbreaks during 2019.
The spread of germs from the hands of food workers to food is an important cause of foodborne illness outbreaks in restaurants. It accounts for 89 percent of outbreaks in which food was contaminated by food workers, reported the CDC on June 18, 2019.
Early diagnosis and medical care are the keys to preventing more serious health outcomes.
"Hepatitis A is a preventable disease through receiving a vaccination, staying up to date with vaccination, and using proper hygiene in the foodservice industry. People in the foodservice industry should check with their local pharmacist to be sure they are up to date with their vaccinations, advised Lauren Ragan, PharmD, Clinical Pharmacist for Brookshire Grocery Company.
Vaccination is recommended for all children starting at 1 year, for travelers to certain countries and for people at high risk for infection. While hepatitis A vaccination has been recommended for children since 2006, many adults have not been vaccinated for hepatitis A.
MDH also has been notifying healthcare providers so they can be alert to test for hepatitis A if a patient has symptoms and so they can provide vaccine if an opportunity occurs, to those at risk of infection.
>> Confidential Hepatitis A Tests <<
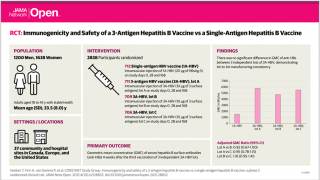
There are 3 HAV vaccines approved in the USA: Vaqta, Havrix, and Twinrix, which are available at pharmacies in most states.
Furthermore, immune globulin can provide short-term protection against hepatitis A, both pre- and post-exposure.
The exact duration of protection after vaccination is unknown. Anti-HAV has been shown to persist for at least 20 years in adults administered inactivated vaccine as children with the three-dose schedule, and anti-HAV persistence of at least 20 years also was demonstrated among persons vaccinated with a two-dose schedule as adults, says the CDC.
More information about Hepatitis A symptoms and prevention can be found on the CDC website. Any hepatitis vaccine can cause side effects, which should be reported to a healthcare provider or the CDC.
Our Trust Standards: Medical Advisory Committee
- Health officials declare hepatitis A outbreak among people with high-risk factors
- CDC: Widespread outbreaks of hepatitis A across the United States
- Health officials declare hepatitis A outbreak among people with high-risk factors
- Health Care Utilization and Associated Costs of Hepatitis A in Adults in a US Commercially Insured Population
- Public Health Impact an Cost-Effectiveness of Hepatitis A Vaccination in the United States: A Disease Transmission Dynamic Mode
- The Cost of Hepatitis A Infections in American Adolescents and Adults in 1997