Should Childbearing Age Women Be Vaccinated Against Zika?

A recent Zika study focused on ‘how best to eliminate the mosquito and sexual transmission of the Zika virus with a preventive vaccine.
These researchers said ‘while vaccinating everyone naturally averted the most possible Zika cases, targeting women of childbearing age, children and young adults with a preventive vaccine was found to be the most cost-effective.’
These researchers said ‘Zika vaccinations could actually pay for itself.’
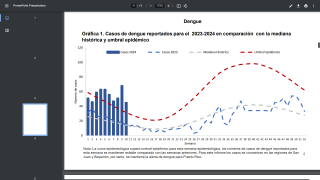
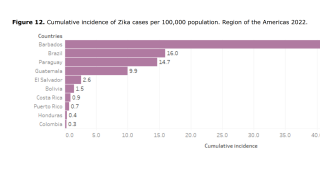
This study published in the Journal of Infectious Diseases (in print September 2019) simulated various vaccination strategies to mitigate Zika outbreaks in Honduras, Brazil, and Puerto Rico.
Theoretically, vaccinating the selective populations of these 3 countries averted about 5.7 million Zika cases and 38,158 Guillain-Barré Syndrome related fatalities.
As an example, a 2018 study found about 43 percent of tested individuals in Puerto Rico were found to be infected with the Zika virus.
And, as of August 1, 2019, there have been 24 Zika cases confirmed in Puerto Rico by the Centers for Disease Control and Prevention (CDC).
While vaccinating everyone could avert direct healthcare costs and productivity losses, vaccination costs were higher, and vaccination did not result in overall cost savings in Honduras or Brazil for a 2 percent virus attack rate.
However, at $5 per vaccination cost, there was saving between $29.7–$46.1 million in societal costs in Honduras, and $0.4–$2.7 billion in direct costs and $3.6–$11.7 billion in societal costs in Brazil for a 20 percent virus attack rate.
A similar vaccination program in Puerto Rico would generate cost savings of $0.1–$126.2 million in direct costs and $1.5–$499.5 million in societal costs, depending on actual Zika vaccine’s characteristics.
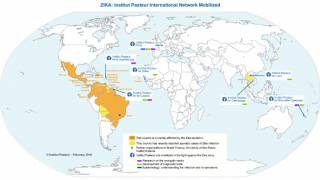
In a related editorial by Hannah E. Clapham, Ph.D. Mathematical Epidemiologist, University of Oxford, said ‘the impact of this from the 2015–2016 Zika epidemics will continue to be felt for many years and continued research support is necessary to understand it.’
‘Though important, protecting against mosquito bites and sexual transmission would appear to be insufficient to completely control Aedes aegypti–borne virus transmission.’
‘Therefore, any available vaccine against the Zika virus would be an important part of effective future control.’
Importantly, the study’s main scenario considered is one in which a Zika outbreak does not happen until 5 years after vaccination started.
‘There are also a number of epidemiological uncertainties to be further considered to fully assess the global cost-effectiveness of Zika vaccination,’ said Dr. Clapham.
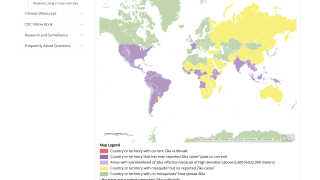
‘Zika is not gone forever.’
‘Mathematical modeling studies like the one reported here can help us understand the future risks, but to understand the epidemiology of Zika moving forward, we also need continued surveillance to identify areas with active virus transmission,’ concluded Dr. Clapham.
According to various reports, there are approximately 45 different Zika virus vaccine candidates at various stages of development with several undergoing phases I and II clinical trials in humans.
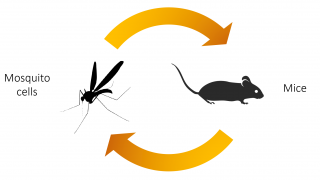
Multiple vaccine platforms, including live attenuated vaccines, chimeric virus vaccines, and RNA vaccines have been tested in pre-clinical mouse pregnancy models:
And, the US Food and Drug Administration has awarded ‘Fast Track’ status to certain Zika vaccine candidates:
In general, most of these vaccines were effective at reducing or preventing vertical transmission of the Zika virus in mice, in terms of reduced infection of the placenta, fetus and/or fetal brain.
However, to date, there has been less extensive testing for their ability to block vertical transmission to the fetus during pregnancy or prevent the development of Congenital Zika Syndrome.
Thus, the challenge for future vaccine development is to determine vaccine efficacy at protecting the fetus when the vaccine is delivered prior to pregnancy and how long such protection persists.
Moreover, guidance is also needed on the conditions under which is it ethically acceptable, if not required, to include pregnant women in Zika vaccine trials.
Dr. Clapham’s editorial was funded by the Wellcome Trust (grant number 089276/B/09/7). The author certifies no reported conflicts of interest. Conflicts that the editor considers relevant to the content of the manuscript have been disclosed.
And the initial study was supported by the Bill & Melinda Gates Foundation (Award Number OPP1139051); Instituto Carlos Slim de la Salud; the National Institutes of Health (grant numbers U01 GM087719, U01 GM105627, U54HD070725, U01 HD086861); the Agency for Healthcare Research and Quality (grant number R01HS023317); and the US Agency for International Development (grant number AID-OAA-A-15-00064)
Our Trust Standards: Medical Advisory Committee
- What Is the Value of Different Zika Vaccination Strategies to Prevent and Mitigate Zika Outbreaks?
- Determinants of Zika Transmission and Control
- How research is helping kids growing up with congenital Zika syndrome
- Intraamniotic Zika virus inoculation of pregnant rhesus macaques produces fetal neurologic disease
- Pregnant Women & the Zika Virus Vaccine Research Agenda: Ethics Guidance on Priorities, Inclusion, and Evidence Generation