Egg-based Flu Vaccines May Deliver Substandard Protection

Health officials in the US are now warning that this season’s flu shot may only be 10% effective.
And the reason may be related to how most flu vaccines are made…. in eggs, as previously reported in November 2017.
Anthony Fauci, M.D., the head of the National Institute of Allergy and Infectious Diseases, and a research team disclosed a forecast that only 10 percent of people will be protected by an egg-based flu shot this season.
This article was published in a New England Journal of Medicine commentary, which is excerpted below.
“As clinicians in the United States prepare for the start of another influenza season, experts have been watching the Southern Hemisphere winter for hints of what might be in store for us in the North.
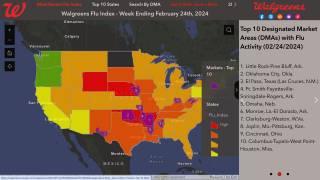
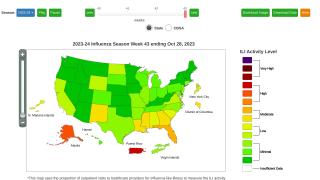
Reports from Australia have caused mounting concern, with record-high numbers of laboratory-confirmed influenza notifications and outbreaks and higher-than-average numbers of hospitalizations and deaths.
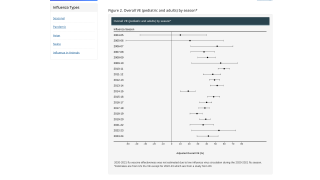
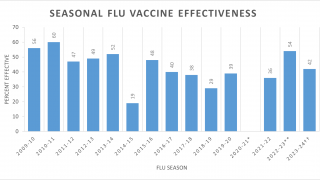
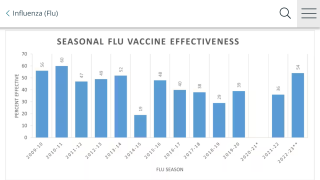
According to the Australian Government Department of Health. Influenza A (H3N2) viruses were predominant. And the preliminary estimate of vaccine effectiveness against influenza A (H3N2) was only 10%.
The implications for the Northern Hemisphere are not clear, but it is of note that the vaccine for this upcoming season has the same composition as that used in the Southern Hemisphere.
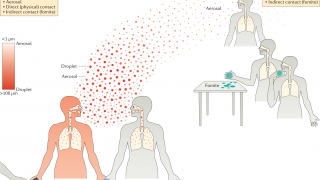
Since influenza viruses are subject to continual antigenic changes (“antigenic drift”), vaccine updates are recommended by the WHO each February for the Northern Hemisphere and each September for the Southern Hemisphere.
Vaccine mismatches have occurred in years in which circulating influenza strains change after the decision is made about vaccine composition, resulting in reduced vaccine effectiveness.
As we prepare for a potentially severe influenza season, we must consider whether our current vaccines can be improved and whether longer-term, transformative vaccine approaches are needed to minimize influenza-related morbidity and mortality.
In the United States, most influenza-vaccine viruses are propagated in eggs, although a small proportion is produced either in cell culture or by expressing specific viral proteins using recombinant DNA technologies.
During the egg-based production process, the vaccine virus acquires amino acid changes that facilitate replication in eggs, notably changes in the hemagglutinin (HA) protein that mediates receptor binding.
Since the influenza HA is the primary target of neutralizing antibodies, small modifications in this protein can cause antigenic changes in the virus and decrease vaccine effectiveness.
Egg adaptation has been postulated to contribute to low vaccine effectiveness, particularly with influenza A (H3N2) viruses; however, the true impact is largely unknown.
Given that most of the U.S. influenza-vaccine supply is currently produced in eggs and the composition of the 2017–2018 Northern Hemisphere vaccine is identical to that used in Australia, it is possible that we will experience low vaccine effectiveness against influenza A (H3N2) viruses and a relatively severe influenza season if they predominate.
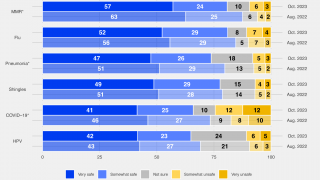
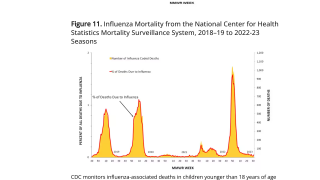
However imperfect, though, current influenza vaccines remain a valuable public health tool, and it is always better to get vaccinated than not to get vaccinated.
In this regard, the CDC estimates that influenza vaccination averted 40,000 deaths in the United States between the 2005–2006 and 2013–2014 seasons.
Yet we can do better.
Starting with the 2017–2018 influenza season in the United States, cell-based vaccines will use cell-based seed strains.
From the Office of the Director, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD (C.I.P., A.S.F.); and the World Health Organization Collaborating Centre for Reference and Research on Influenza, Peter Doherty Institute for Infection and Immunity, Melbourne, VIC, Australia (S.G.S., K.S.).
Contact Jennifer Routh, 301-402-1663, [email protected] Author Disclosure forms provided by the authors are available at NEJM.org.
Our Trust Standards: Medical Advisory Committee