Pneumonia Antibiotic Therapy Fails for 22% of Patients
Approximately 22 percent of adults prescribed an antibiotic in an outpatient setting did not respond to treatment, according to a new study presented at the 2017 American Thoracic Society International Conference.
This data indicates prescribing guidelines may need to be updated.
"Our data provide numerous insights, such as patients over the age of 65 were nearly twice as likely to be hospitalized compared to younger patients and nearly three times more likely in unadjusted analysis," said lead author James A. McKinnell, MD, an LA BioMed (Los Angeles, CA) lead researcher and infectious disease specialist.
In addition, this study showed that thousands of patients who suffer from other conditions, such as chronic obstructive pulmonary disease (COPD), cancer, or diabetes, were not treated with combination antibiotic therapy or a respiratory fluoroquinolone, as the guidelines recommend.
"While certain aspects of the guidelines need to be updated, some prescribers also have room for improvement and should implement the current guidelines," Dr. McKinnell concluded.
"Pneumonia is the leading cause of death from infectious disease, so it is concerning that we found nearly one in four patients with community-acquired pneumonia required additional antibiotic therapy, subsequent hospitalization or emergency room evaluation," said Dr. McKinnell.
"The additional antibiotic therapy noted in the study increases the risk of antibiotic resistance and complications like C. difficile ("C diff") infection, which is difficult to treat and may be life-threatening, especially for older adults," said Dr. McKinnell.
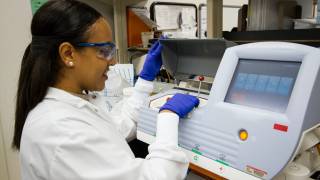
The researchers examined databases containing records for 251,947 adult patients who were treated with a single class of antibiotics (beta-lactam, macrolide, tetracycline, or fluoroquinolone) following a visit to their physician for treatment for community-acquired pneumonia.
These scientists defined treatment failure as either the need to refill antibiotic prescriptions, an antibiotic switch, ER visit, or hospitalization within 30 days after starting the initial antibiotic therapy.
The total antibiotic failure rate was 22.1 %. Patients with certain characteristics, such as older age, or having certain other diseases in addition to pneumonia, had higher rates of drug failure.
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for all babies and children younger than 2 years old and all adults 65 years or older. Pneumococcal vaccines are vaccines against the bacteria Streptococcus pneumoniae. Their use can prevent some cases of pneumonia, meningitis, and sepsis.
There are 2 types of pneumococcal vaccines: conjugate vaccines and polysaccharide vaccines. They are given either by injection into a muscle or just under the skin.
There is no evidence on the safety of Prevnar13 use during pregnancy. As a precaution, women who need the vaccine should be vaccinated before becoming pregnant, if possible.
Prevnar 13® is a leading vaccine approved for adults 18 years of age and older for the prevention of pneumococcal pneumonia and invasive disease caused by 13 Streptococcus pneumoniae strains. Prevnar 13® is not 100% effective and will only help protect against the 13 strains included in the vaccine.
If a person needs help paying for Pfizer medicines, such as Prevnar 13, they can learn more at PfizerRxPath.com.
Pneumococcal vaccines are available at pharmacies, workplaces, community health clinics, health departments, or other community locations such as schools and religious centers.
The CDC Vaccine Price Lists posted on this website provide current vaccine contract prices and list the private sector vaccine prices for general information.
These authors did not disclose any conflicts of interest: J. McKinnell, P. Classi, P. Blumberg, S. Murty, G. Tillotson.
Our Trust Standards: Medical Advisory Committee