Herpes Vaccine Candidates Need to ‘Wake Up CD8 T-Cells’

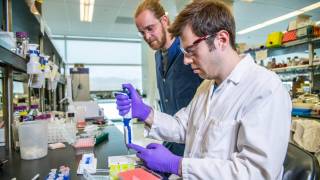
Researchers have shown in a new study how a skin vaccination can generate protective CD8 T-cells that are recruited to the genital tissues and could be used as a vaccination strategy for sexually transmitted infections (STIs).
This is good news since there is not a commercially available herpes simplex virus vaccine available today.
One of the challenges in developing vaccines for STIs, herpes simplex virus, is understanding how to attract specialized immune cells, called CD8 T-cells, to take up residence in the part of the body where the virus first enters.
These CD8 T-cells need to be in place, armed and ready to provide an immediate protective immune defense, rather than waiting for immune cells in the blood to enter the tissues which takes time, said these School of Immunobiology and Microbial Sciences researchers, at King's College London, in a May 17, 2019, press release.
Before this new study published in Nature, it was thought that vaccines ideally needed to be delivered directly to the body surface (e.g. female genital tissue) where the infection might start, so that the immune system can generate these CD8 T-cells, travel back to the vaccination site and eliminate any future virus that is encountered.
However, delivering vaccines directly to the female genital tissue is neither patient-friendly nor efficient.
Now the team from King's have found that their vaccination strategy marshals a platoon of immune cells, called innate lymphoid cells (ILC1) and monocytes, in the genital tissues to work together and release chemicals known as chemokines, to send out a call to the CD8 T-cells generated by the vaccine to troop into the genital tissue.
Lead author, Professor Linda Klavinskis from King's College London said, "This study highlights how specialized groups of 'innate' immune cells in distant tissues can be harnessed to attract protective CD8 T-cells, arming the body's frontline tissues from infection.”
In conclusion, ‘we have defined a mechanism whereby skin vaccination induces low-level inflammation in the FRT that is sufficient to promote CD8+ T-cell recruitment through a CXCL9-dependent mechanism licensed by ILC1 cells.’
‘These data may have important implications for vaccine designs against pathogens transmitted across epithelial barrier tissues and highlight the attributes of the skin as a delivery site to stimulate prophylactic and therapeutic immunity against vaginally acquired infections.’
"We now need to confirm these results with other types of vaccines to see if a common pathway is triggered by skin vaccination.”
“If proven, this could have a significant impact in improving the effectiveness of vaccines against sexually transmitted infections," said Dr. Klavinkis.
This work was funded by The Bill and Melinda Gates Foundation, Seattle, WA grant number 38639 and European Union Marie Curie Initial Training Network (UniVacFlu) grant number 607690 to LSK and grants BB/L027933/2 and CH/11/2/28733 to AHB.
No conflicts of interest were disclosed by these Kings College London researchers.
Our Trust Standards: Medical Advisory Committee