Cervical Cancer Prevention Starts With Screening and Vaccinations

Women are being asked to make a New Year’s resolution to talk with their healthcare providers about cervical cancer prevention, says the National Cervical Cancer Coalition (NCCC).
Nearly 13,000 women in the United States are diagnosed with cervical cancer each year, but the disease is preventable with vaccination and screening, such as Pap and HPV tests, said the NCCC in a press release.
“When cervical cancer is found early, it is highly treatable,” said Dr. Sarah Ramirez, a family medicine physician with Penn State Health.
“So it’s important to make sure women are being screened for this disease.”
While many women are still suffering and dying from it, cervical cancer incidence is on a downward trajectory.
Cervical cancer is no longer the leading cancer caused by human papillomavirus (HPV).
That’s because Gardasil 9, a vaccine that prevents certain cancers and diseases caused by the 9 HPV types, is now available, Dr. Ramirez said in a Penn State Health statement.
And now, more people have access to Gardasil.
In October 2018, the U.S. Food and Drug Administration approved the application of Gardasil 9 to include both women and men younger than 45 years old, and older than 8 years of age.
“Our mindset should shift from seeing Gardasil as a vaccine that prevents a sexually transmitted disease related to cancer. Instead, we should see it as a cancer prevention tool.”
“This approval speaks to the power of the vaccine to prevent cancer,” Dr. Ramirez said.
But testing and early detection remain an important key to prevention, and many are still at risk.
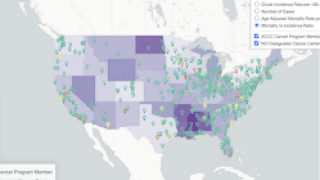
“As the U.S. population becomes increasingly diverse, it behooves us to examine why there is a disparity in cervical cancer health with our vulnerable populations and why they’re not getting screened regularly,” Dr. Ramirez said.
Hispanic or Latina women get fewer Pap tests than non-Hispanic white and black women, even though Hispanics have the highest incidence of cervical cancer, according to the American Cancer Society Cancer Action Network.
Similarly, African American females have the highest rate of death due to cervical cancer, according to the Centers for Disease Control and Prevention (CDC).
Waiting for the disease to show itself can be risky.
According to the United States Preventive Services Task Force, all women between 21 and 65 years of age should have cervical cancer screening with cytology (Pap smear) every 3 years.
Women between the ages of 30 and 65 may opt instead to lengthen the interval between screening with a combination of cytology and HPV testing every five years.
A third option for women, 30 to 65, is to choose to get screened every 5 years with HPV testing alone.
HPV is a group of more than 150 related viruses. Each HPV virus in this large group is given a number which is called its HPV type, says the Centers for Disease Control and Prevention (CDC).
HPV is passed from one person to another during sex, and at least half of sexually active people will have HPV at some point in their lives, even though relatively few women will develop cervical cancer.
HPV cancers include cancer of the cervix, vulva, vagina, penis, or anus. An HPV infection can also cause cancer in the back of the throat, including the base of the tongue and tonsils.
HPV vaccines can be found in most authorized pharmacies and physician offices in the USA.
To schedule a vaccination appointment, please visit this page.
The CDC Vaccine Price List provides HPV vaccine prices for general information. And vaccine discounts can be found here.
Vaccines, like any medicine, can have side effects, says the CDC. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee