UK Mandates 6-in-1 Vaccination for Infants

It’s hard to imagine putting your newborn infant through the pain of another vaccination. So the United Kingdom’s National Health Service (NHS) will soon offer the Hepatitis B to infants before they leave the hospital.
This new policy, which takes effect in August, 2017, acts as a safety net, as the Hepatitis B immune globulin (HBIG) gives an infant extra help to fight the virus as soon as possible.
Currently, the HepB vaccine is available to children as a separate vaccination, offered to high risk children, such as those born to infected mothers. Pregnant women have a routine blood test for HepB as part of their prenatal care.
The change aligns the UK with other EU countries. The World Health Organisation (WHO) recommended in 1992 that infants should be immunized against the HepB virus.
HepB protects people from viral infections which cause cirrhosis and liver cancer.
The HepB vaccine will be added to the 5-in-1 protocol, which is already given to newborn infants in the UK to protect them from diphtheria, tetanus, whooping cough, polio and haemophilus influenzae type B. The 5-in-1 vaccine is a single injection.
According to the WHO, infants born to mothers found to be infected with hepatitis B need to be given a dose of the hepatitis B vaccine within 24 hours of their birth, followed by further doses at 1, 2 and 12 months old.
As soon as a baby is born they come into contact with a huge number of different bacteria and viruses every day, and their immune system copes with them and becomes stronger as a result.
Hepatitis B is a liver infection caused by a virus that is spread through blood and bodily fluids. In many adults, the infection does not cause obvious symptoms and typically clears up in a few months without treatment.
But in children the virus can linger for years and cause serious liver damage.
The infection is less common in the UK than other parts of the world, but certain groups are more at risk than others. Most infections in the UK are found in people who inject drugs and those who have unprotected sex with multiple partners.
In WHO regions Asia and the Pacific Islands, 10% or more of the population have chronic hepatitis B infections.
The first ever WHO Global Hepatitis Report was published in June 2017, and offered some good news and some bad news.
According to this new report, an estimated 1.34 million people died from hepatitis in 2015. This is higher than the number of deaths caused by AIDS. Additionally, about 328 million people were believed to have active hepatitis infections as of 2015.
The WHO reports that 84% of children born in 2015 received the 3 recommended doses of the hepatitis B series. However, only 1/3 of children worldwide are receiving the first dose of the vaccine at birth.
This leaves a window of risk that allows for new infections.
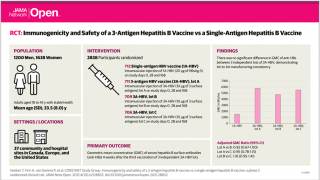
Vaccines for hepatitis B virus (HBV) were first released in 1982. The Centers for Disease Control and Prevention (CDC) began recommending infant immunization in the USA in 1991. According to the CDC, individuals who become infected with hepatitis may not know they have the disease.
Without a diagnosis, there’s no treatment. Without treatment, there’s no stopping the spread of hepatitis B. Furthermore, when the virus does make itself known, whether through liver damage or liver cancer, the disease is too advanced for treatment.
For patients not covered by insurance, the total cost of a hepatitis vaccination usually includes shot administration fees.
The CDC current vaccine contract prices can be found here.
Our Trust Standards: Medical Advisory Committee