Last Season's Influenza Virus Changed Personalities

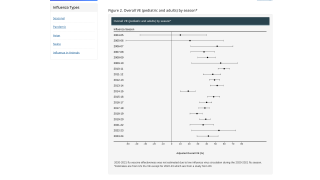
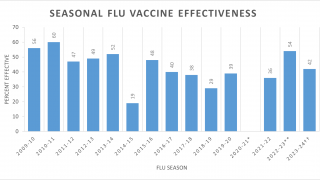
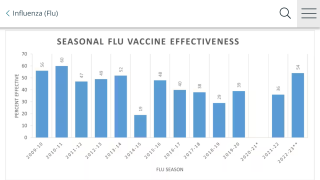
A new study found the predominance of A(H3N2) clade 3C.3a viruses during the latter part of the 2018-2019 Northern Hemisphere influenza season was associated with decreased vaccine effectiveness (VE).
This study’s finding published on October 30, 2019, supports the A(H3N2) vaccine component update for 2019-2020 flu shots.
These Centers for Disease Control and Prevention (CDC) researchers focused on why the 2018-19 flu season was unusual.
The 2009 H1N1 virus predominated during the 1st part of the season, with low levels of H3N2 that was similar to the vaccine component.
The 2018-19 VE was found to be 44 percent against 2009 H1N1 viruses and just 9 percent against H3N2 viruses.
Which is good news.
Then, during the latter part of the last flu season in 2019, a ‘drifted H3N2 variant emerged from the 3C.3a clade,’ which decreased the flu vaccine’s effectiveness to just 5 percent.
And VE for any H3N2 strain did not rise to the level of statistical significance.
These CDC researchers used the U.S. virologic surveillance and Influenza Vaccine Effectiveness (VE) Network data to evaluate the consequences of this clade.
The VE Network enrolled ambulatory patients aged ≥6 months with acute respiratory illness at 5 sites. Respiratory specimens were tested by RT-PCR for influenza and sequenced.
Using a test-negative design, they estimated VE comparing odds of influenza among vaccinated versus unvaccinated participants.
In a related commentary, Robert Atmar, M.D., and Wendy Keitel, M.D., from Baylor College of Medicine in Houston, Texas, acknowledged that flu shot development is an ongoing challenge in both the Northern and Southern Hemispheres.
These Baylor physicians said ‘the low VE observed against H3N2 strains compared to H1N1pdm09 or B strains this past season is not a new phenomenon.’
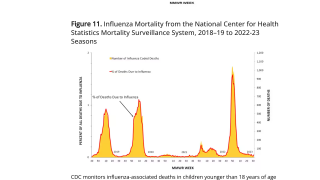
Influenza A and B viruses cause seasonal epidemics between late fall and early spring annually in the United States. Disease impact between the 2010-2011 and 2017-2018 seasons has been estimated to range from 9.2 to 47.9 million illnesses, 1.2 to 22.1 million outpatient medical visits, 139 to 953 thousand hospitalizations and up to 79.4 thousand fatalities each year.
To jump-start flu shot innovation, the National Institute of Allergy and Infectious Diseases (NIAID) recently initiated the Collaborative Influenza Vaccine Innovation Centers (CIVICs) program on September 30th, 2019.
This new network of research centers will work together in a coordinated, multidisciplinary effort to develop more durable, broadly protective and longer-lasting influenza vaccines. The NIAID is providing up to approximately $51 million dollars in total first-year funding for the program, which is designed to support the CIVICs program centers over the next 7-years.
But, the news for the 2020 flu season has not been very positive, such as the following articles:
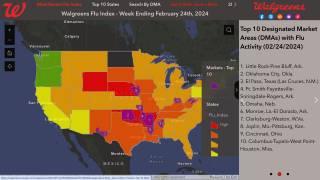
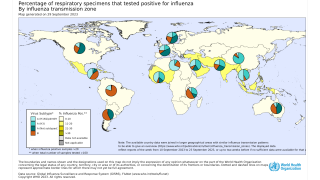
- October 30, 2019 – Seasonal influenza A viruses continued to account for the majority of detections around the globe, though the proportion of influenza B viruses increased in recent weeks, reported the World Health Organization (WHO). Of the 5,005 samples evaluated during early October, influenza A made up 60.5 percent. Of the sub-typed influenza A viruses, 35.6 percent were influenza A(H1N1)pdm09 and 64.4 percent were influenza A(H3N2). Of the characterized B viruses, 85.9 percent to the B-Victoria lineage.
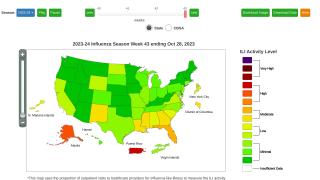
- October 26, 2019 - the CDC reported the seasonal influenza activity in the USA increased slightly, but remains low, when compared to previous years.
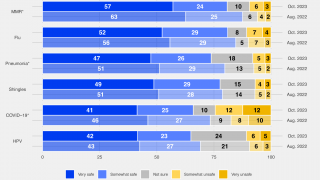
The CDC says everyone 6 months of age and older should get a flu vaccine every season, with rare exceptions. Different flu vaccines are approved for use in different groups of people.
There are flu shots approved for use in children as young as 6 months of age and flu shots approved for use in adults 65 years and older.
Additionally, the CDC continues to recommend that pregnant women get a flu shot during any trimester of their pregnancy because influenza poses a danger to pregnant women.
Influenza vaccines are given during pregnancy to protect both the mother and her baby from influenza. Furthermore, a flu shot reduces the risk of influenza-associated acute respiratory infection in pregnant women by about 50 percent, says the CDC.
Previously, for the first time, the American Lung Association, the American Diabetes Association (ADA), and the American Heart Association (AHA) have come together to raise an important alert about the dangers of the influenza virus.
These associations, in an October 16, 2019 statement, are ‘urging the 117 million adults living with chronic health conditions, including diabetes, heart disease, and lung diseases to prioritize annual flu shots within their practices.’
This new study was published in the Journal of Infectious Diseases on October 30, 2019. No conflicts of interest were disclosed.
As always, vaccination decisions should be part of an ongoing discussion between provider and patient.
Influenza news published by Precision Vaccinations.
Our Trust Standards: Medical Advisory Committee