Moores Cancer Center Testing Personalized Cancer Vaccine
A first-of-its-kind, phase 1 clinical study is testing a personalized vaccine using a person's unique cancer mutations to boost an anti-tumor immune response.
Led by Stephen Schoenberger, Ph.D., professor of immunology at the La Jolla Institute for Allergy and Immunology (LJI), and Ezra Cohen, MD, professor of medicine at the University of California San Diego School of Medicine, scientists and clinicians have developed a technology that reliably defines the neoantigens in a patient’s cancer.
With neoantigens, which are foreign protein fragments recognized by the immune system, identified, the research team can identify peptides that can be used to create a vaccine to stimulate a protective immune system response.
This means the information in a patient’s cancer is used to boost the immune system to initiate a stronger response from both cytotoxic and “helper” T cells — white blood cells that collaborate to destroy cancer cells.
“T cells need to recognize a cancer cell as being different before they can produce a response to destroy a patient’s tumor,” said Dr. Cohen in a press release.
“It’s a complicated process to harness this power into a vaccine.”
“We are creating an incredibly personalized and precise therapy that is based on what that person’s cancer and immune system are telling us. Each vaccine we develop only applies to a specific individual,” said Dr. Cohen.
Dr. Schoenberger and LJI’s Bjoern Peters, Ph.D., developed a novel algorithm to select mutations that are recognized by the immune system. This algorithm was deployed to recognize the neoantigens that generated the strongest T cell response from a patient’s tissue samples.
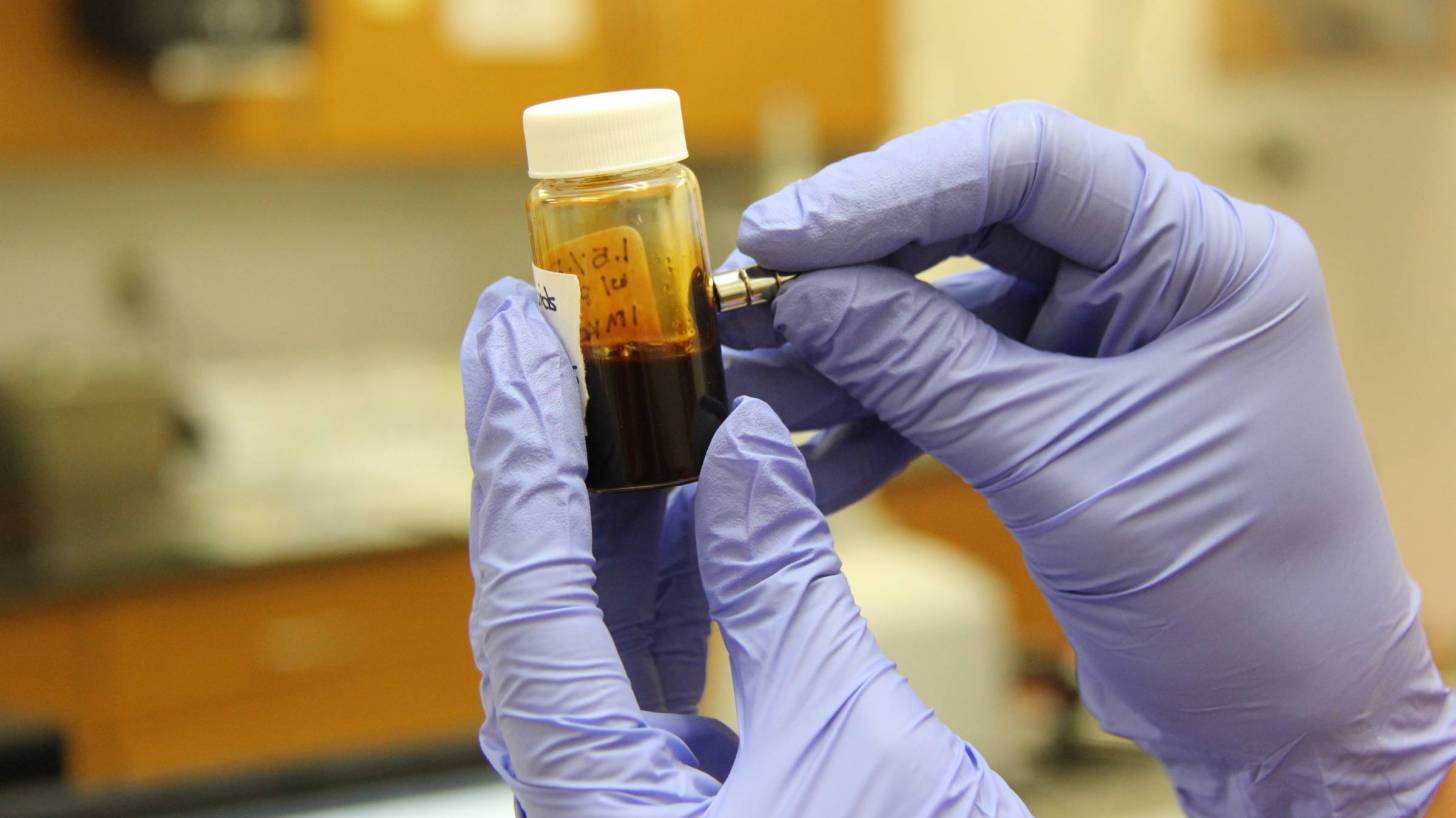
These neoantigens were then presented to the patient’s own T cells and cultured over a two-week period using 50 milliliters of their blood to develop a personalized vaccine.
“It's been invention and new science every step of the way. This process simply hasn't existed until we tried to build it here,” said Dr. Schoenberger.
“By opening up our eyes and measuring what's really happening with the cancer cells and the immune system, rather than predicting what we hope is there, we could make the transformational step needed to make this approach possible.”
The vaccine is part of a one-two punch.
In addition to the vaccine, patients receive pembrolizumab (Keytruda), an FDA-approved immune checkpoint blockade inhibitor that blocks the abnormal interaction between the molecule PD-1 on immune cells and the molecule PD-L1 on cancer cells, allowing the immune cells to recognize and attack tumors.
Combined with the vaccine, the drug should unleash the full potential of T cells activated by the vaccine, said Dr. Schoenberger.
During this very limited trial, participants will return for 2 additional vaccine doses and remain on pembrolizumab for up to two years. Their health will be monitored for a minimum of 5 years.
Our Trust Standards: Medical Advisory Committee



























