Innovative Vaccine Technologies Help Respond to Emerging Viral Diseases
Novel vaccine technologies are critical to improving the response to infectious disease threats, according to scientists at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH).
In a perspective published in The Journal of the American Medical Association, these experts highlight innovations that could significantly shorten the typical decades-long vaccine development timeline.
Historically, vaccines against viral diseases have used live-attenuated (weakened) viruses or inactivated whole viruses to induce protective immune responses.
This development process often takes 15 to 20 years or more and requires virus cultivation, animal model testing, product formulation, immunogenicity testing and years of costly clinical trials.
Fortunately, during the last decade, there have been substantial technological advances for conceiving, developing, manufacturing, and delivering vaccines.
Technological advances such as synthetic vaccinology and platform manufacturing, can expedite the process and shorten manufacturing time, allowing clinical evaluation to begin sooner, according to the authors.
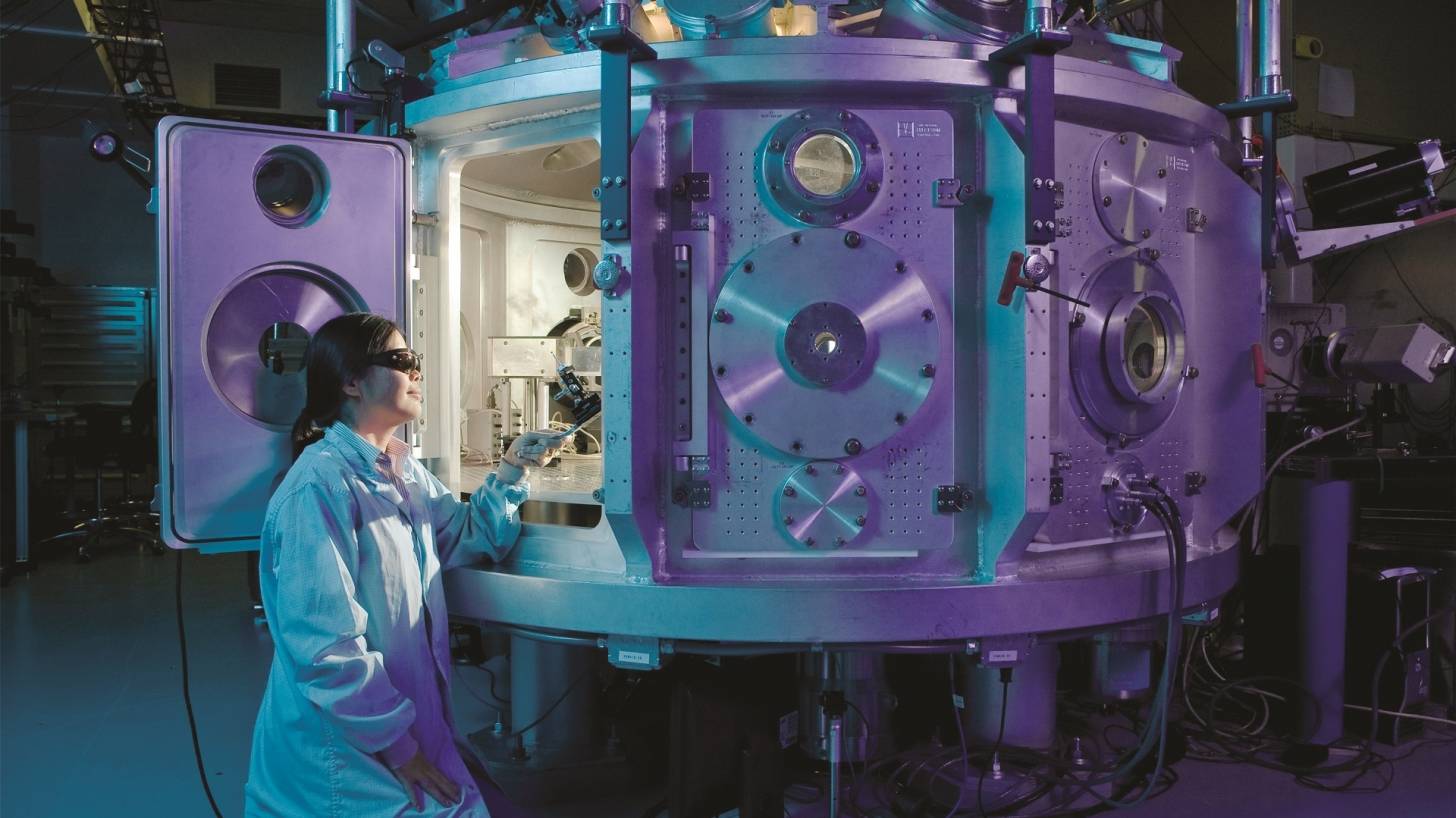
Synthetic vaccinology uses information from viral gene sequencing to create DNA and mRNA molecules encoding viral proteins.
Because this research does not require replicating “live” viruses, it does not need to be done in high-level containment facilities when developing vaccines for highly pathogenic viruses.
The perspective notes that once a vaccine platform is established, such as that for DNA or mRNA vaccines, potentially it can be applied to multiple pathogens, especially within virus classes or families.
For example, NIAID’s Vaccine Research Center quickly developed a candidate DNA vaccine for Zika virus with the same platform used previously for a related flavivirus, West Nile virus.
Platform technologies enable scientists to apply a standardized manufacturing process to multiple vaccines and create a collective database on their safety as well, which can shorten the preclinical development period to as little as several months, according to these authors.
The perspective concludes that modern vaccine technology and improved surveillance in developing countries ultimately can help us better prepare for emerging infectious disease threats.
Rapid genetic sequencing allows both early identification of new pathogens and the identity of the genes encoding structural proteins that can form the basis for vaccine immunogen development.
Also, rapid isolation of human monoclonal antibodies has proven to be extremely helpful in defining epitopes that are the targets of protective immunity.
Additional tools of modern vaccinology include:
- delineation of atomic-level structures of viral proteins that facilitates structure-enabled immunogen design and protein engineering;
- cell sorting and sequencing technologies that allow single-cell analysis of immune responses; and,
- genetic knock-in technologies that allow construction of animal models with human antibody genes for vaccine testing.
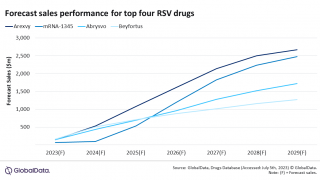
These tools have already provided the potential not only for solving long-standing problems in vaccinology, such as the development of a new candidate vaccine for respiratory syncytial virus.
Additionally, they have facilitated rapid development of new candidate vaccines for emerging pathogens such as the Zika virus and pandemic strains of influenza virus.
Synthetic vaccinology and platform manufacturing are important innovations that can speed the initial vaccine immunogen design and vaccine development process, and shorten the time needed for manufacturing and initial regulatory approval to begin phase 1 testing.
Similarly, if an outbreak of a new flavivirus becomes an epidemic or even a pandemic threat, as with Zika in 2015, the gene sequences that encode the viral surface proteins pre-membrane and envelope can be rapidly identified and form the basis for vaccine immunogen design strategies, based on prior knowledge of flavivirus structure and mechanisms of neutralization.
Once a structurally authentic immunogen is available, the protein or genetic vectors encoding the protein can be used to immunize animals.
In addition, the vaccine proteins can be used as probes to identify monoclonal antibodies secreted by B cells of convalescent humans.
Such antibodies are valuable not only for refining vaccine immunogen designs but also for the development of diagnostic assays and potentially for use in passive transfer as therapeutic agents.
Thus, development of reagents, diagnostics, candidate vaccines, and immune assessment assays can be done without having the actual virus in hand.
This has particular value for viruses with extreme pathogenicity because it avoids the need for high-level containment in laboratory and manufacturing facilities.
In summary, emerging viral diseases with pandemic potential are a perpetual challenge to global health.
To effectively prepare for and respond to these continually emerging threats, it will be critical to exploit modern-day technological advances, preemptively establish detailed information on each family of viral pathogens, and invest in more infrastructure for surveillance in developing countries to expedite pathogen identification and jump-start the process of vaccine development using these new technologies.
Failure to do so will result in the untenable situation of not optimally using vaccinology in the response to newly emerging infectious disease threats.
Corresponding Author: Anthony S. Fauci, MD, Laboratory of Immunoregulation, National Institute of Allergy and Infectious Diseases, 31 Center Dr, MSC 2520, Bldg 31, Room 7A-03, Bethesda, MD 20892-2520 ([email protected]).
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Drs Graham and Mascola reported they are inventors on a pending patent application for a Zika DNA vaccine for which a licensing agreement is being negotiated.
Our Trust Standards: Medical Advisory Committee